Ovarian Cancer Causes: Essential Risk Factors Every Woman Should Know
Introduction
Many women don’t recognize symptoms of ovarian cancer until the disease has already advanced, which is why it is often called a “silent” or “concealed” illness. For many women globally, understanding not just what ovarian cancer is, but also its causes and the individuals most at risk, is crucial. Gaining insight into significant causes and risk factors is a vital first step towards early detection, making informed health decisions, and pursuing proactive medical screening.
Though physicians and researchers have yet to pinpoint a single definitive cause of ovarian cancer, various genetic, hormonal, reproductive, and lifestyle factors can greatly impact a woman’s risk. Some women carry inherited genetic mutations that elevate their odds of developing the disease, while others might experience heightened risk due to factors like age, menstrual history, infertility, or existing health conditions. Often, risk factors are not immediately apparent—emphasizing the importance of awareness.
In this guide, we will outline the primary established and emerging risk factors linked to ovarian cancer, elucidate how they influence the body, and dispel common myths versus medical truths. Whether you’re looking to assess your personal risk or stay informed, this article will equip you with the knowledge necessary for making informed health decisions and knowing when to seek medical consultation.
What Is Ovarian Cancer? (Brief Overview)
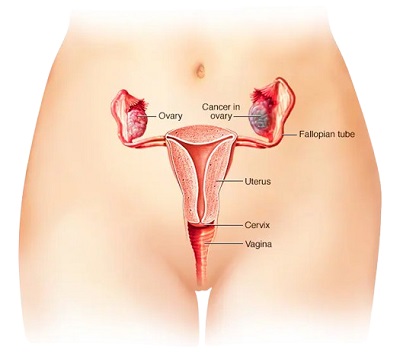
Ovarian cancer develops within the ovaries, the female reproductive organs responsible for producing eggs and hormones like estrogen and progesterone. The disease arises when abnormal cells in the ovary grow and multiply uncontrollably, forming a tumor that can invade adjacent tissues or spread to other body regions if not detected early.
Epithelial ovarian cancer, which originates in the thin tissue layer covering the ovary, is the most common type. Less frequently, germ cell tumors (which stem from egg-producing cells) and stromal tumors (arising from hormone-producing tissue) can occur. Each type behaves uniquely and may necessitate different diagnostic and treatment approaches.
Ovarian cancer’s seriousness stems from its tendency to develop with few early, noticeable symptoms. Therefore, doctors diagnose many cases later, when treatment is more complex. Understanding the disease’s development—along with its causes and risk factors—is crucial for enhancing awareness, facilitating early evaluation, and improving health outcomes.
The Importance of Understanding Ovarian Cancer Causes
Gaining insight into the causes and risk factors of ovarian cancer transcends mere medical knowledge—it empowers women to take charge of their health. Knowing the risk factors can help women recognize when they might need screenings, lifestyle changes, or medical consultations because ovarian cancer often develops subtly and doctors often diagnose it at later stages.
Awareness of potential causes also aids in early risk assessment. Women with a robust family history, genetic mutations, reproductive risk factors, or specific medical issues can engage with their healthcare provider about preventive strategies, including genetic testing or more frequent monitoring. Early identification of high-risk individuals can drastically enhance outcomes.
Moreover, understanding risk factors separates facts from myths. Many women fret about unfounded causes while overlooking established medical risks such as age, genetics, and hormonal history. Evidence-based awareness empowers women to make sound decisions concerning contraception, fertility treatments, hormone therapy, weight management, and general lifestyle choices.
Ultimately, awareness of ovarian cancer causes fosters proactive health behaviors—encouraging regular checkups, attentiveness to bodily changes, and seeking professional evaluation when symptoms or risks are present.
Key Proven Risk Factors and Possible Causes of Ovarian Cancer
While no single confirmed cause for ovarian cancer exists, studies indicate that certain factors can heighten a woman’s likelihood of developing the disease. These risk factors might be genetic, hormonal, reproductive, lifestyle-related, or linked to underlying health conditions. Recognizing these does not imply that a woman will definitely develop ovarian cancer—rather, it aids in identifying those who may need closer surveillance or preventive care.
4.1 Genetic and Family History Factors
Genetics plays a crucial role in ovarian cancer susceptibility.
– Mutations in the BRCA1 and BRCA2 genes significantly heighten risks for both ovarian and breast cancer.
– Lynch syndrome (hereditary non-polyposis colorectal cancer) is also associated with elevated ovarian cancer chances.
– Women with familial ties (mother, sister, daughter, or grandmother) who have faced ovarian, breast, or colorectal cancer encounter a greater lifetime risk.
Women with a notable family history may benefit from:
– Genetic counseling
– BRCA testing
– Risk-reduction strategies suggested by healthcare professionals
4.2 Age and Menstrual History
The risk increases with age, particularly post-40, with the majority of cases occurring after menopause. Some reproductive patterns slightly increase the risk.
– Early menstruation (before age 12)
– Late menopause (after age 52)
– Higher lifetime ovulation cycles
This aligns with the “ovulation theory,” proposing that repeated ovulation may lead to cellular alterations in ovarian tissue over time.
4.3 Reproductive and Pregnancy Factors
Women who have never been pregnant or experience their first pregnancy later in life may experience higher risks than those who have had multiple pregnancies. Additional considerations include:
– Some studies suggest infertility and treatments that stimulate ovulation might correlate with risk, though findings remain mixed and under review.
– Breastfeeding and oral contraceptives appear to lower risks by minimizing lifetime ovulation.
4.4 Hormonal and Medical Factors
Hormonal exposure and specific medical conditions may impact risk.
– Hormone replacement therapy (HRT) — especially prolonged estrogen-only therapy post-menopause — can potentially increase risks.
– Endometriosis has been associated with a higher likelihood of certain ovarian cancer types.
– Conditions such as PCOS (polycystic ovary syndrome) may also correlate with risk, due to hormonal imbalances, weight gain, and metabolic changes.
Women considering HRT should evaluate benefits and risks with healthcare providers.
4.5 Lifestyle and Environmental Risk Connections
While lifestyle choices do not directly “cause” ovarian cancer, they can influence overall risk levels.
– Obesity and excess body weight—especially after menopause—increase the risk.
– Smoking may elevate risk for specific ovarian cancer subtypes.
– Ongoing studies are examining potential exposure to environmental toxins and pollutants.
Maintaining a healthy lifestyle bolsters overall reproductive and metabolic well-being.
4.6 Other Emerging and Suspected Risk Factors
Researchers are exploring additional influences, including:
– Use of talcum powder in the genital area — an ongoing scientific debate with mixed findings; many experts recommend caution.
– Chronic inflammation in pelvic or reproductive tissues
– Immune system responses and inflammation
These fields remain under active investigation, with findings continuing to evolve.

Factors That May Reduce the Risk of Ovarian Cancer
Research also indicates specific factors and lifestyle choices that could help to diminish the overall risk of ovarian cancer, even though it cannot always be averted. While these do not guarantee protection, they could potentially lower the likelihood of developing the disease over a lifetime.
5.1 Use of Birth Control Pills (Oral Contraceptives)
Women utilizing oral contraceptives for several years typically exhibit a reduced risk of ovarian cancer. The reduction in ovulation cycles, which these contraceptives facilitate, is believed to be the source of this protective effect.
– The longer the duration of use, the more substantial the potential protective benefit.
– However, oral contraceptives may pose other health risks, so discussions with a healthcare provider are advisable before making decisions.
5.2 Pregnancy and Breastfeeding
Pregnancy and breastfeeding may contribute to a decreased risk of ovarian cancer by temporarily halting ovulation, leading to less cellular stress on ovarian tissue.
– Having multiple full-term pregnancies could enhance this protective effect.
– Extended breastfeeding may also provide extra benefits for some women.
5.3 Tubal Ligation or Hysterectomy (Medical Context Only)
Certain medical interventions for different health issues might also lower risk:
– Tubal ligation (securing the fallopian tubes)
– Hysterectomy (removal of the uterus, occasionally with the fallopian tubes)
These procedures should not be conducted solely for cancer prevention unless advised for high-risk individuals.
5.4 Healthy Weight and Lifestyle Choices
Maintaining a healthy weight, engaging in physical activity, and limiting smoking and alcohol consumption can help mitigate risk and support hormonal and metabolic well-being.
– Balanced nutrition and effective weight management
– Regular exercise
– Avoidance of tobacco
While lifestyle modifications cannot prevent ovarian cancer entirely, they contribute to improved long-term health outcomes.
5.5 Genetic Counseling and Risk-Reduction Strategies
Women with a significant family history or recognized genetic mutations may find value in:
– Genetic counseling and testing (e.g., assessing BRCA genes)
– Tailored screening plans
– Risk-reducing medical advice from specialists
Identifying hereditary risk early enables proactive monitoring and informed choices.
Myths vs Facts About Ovarian Cancer Causes
Misinformation surrounding ovarian cancer can evoke unnecessary anxiety or lead women to disregard actual medical risk factors. Distinguishing myths from established facts is crucial for informed health choices.
Myth 1: “Ovarian cancer is the result of something a woman did wrong.”
Fact: Most women who develop ovarian cancer have no identifiable controllable cause. Many risk factors—like age, genetics, and family history—are beyond one’s control. While lifestyle choices may influence risk, they do not directly “cause” the disease.
Myth 2: “No family cancer history means I’m not at risk.”
Fact: Although family history elevates risk, most ovarian cancer cases arise in women without any family background of the disease. Every woman has a baseline risk, particularly after midlife.
Myth 3: “Birth control pills raise the risk of ovarian cancer.”
Fact: Studies indicate that oral contraceptives may lower the risk of ovarian cancer by decreasing lifetime ovulation. However, they can pose other health considerations that warrant discussion with a healthcare professional.
Myth 4: “Talcum powder usage always results in ovarian cancer.”
Fact: Research on talcum powder has yielded mixed and inconclusive findings. Some studies suggest a potential correlation, while others do not establish a clear connection. Medical professionals generally recommend caution, but this area remains under scientific examination.
Myth 5: “Ovarian cancer presents early symptoms.”
Fact: Early symptoms are often mild or easily overlooked, resulting in many cases being diagnosed at advanced stages. Persistent bloating, pelvic discomfort, frequent urination, or unexplained abdominal changes should not be dismissed.
Understanding verified information versus speculation empowers women to prioritize genuine health concerns and seek appropriate medical guidance when necessary.

When to See a Doctor
Since ovarian cancer can manifest with subtle or nonspecific symptoms, it’s vital to monitor any changes in your body—especially those that are new, persistent, or worsening over time. Seeking medical advice early does not imply something is severely wrong; rather, it ensures timely assessment and peace of mind.
Key Symptoms That Require Medical Attention
Consult a healthcare provider if you experience any of the following symptoms for longer than two weeks:
– Persistent abdominal bloating or swelling
– Pelvic or lower abdominal discomfort or pressure
– Loss of appetite or feeling uncomfortably full
– Frequent or urgent urination
– Unexplained fatigue, back pain, or digestive alterations
– Abnormal vaginal bleeding (especially post-menopause)
These symptoms do not automatically indicate ovarian cancer, but they warrant thorough evaluation.
Importance of Early Evaluation
Early consultation enables your doctor to:
– Review personal medical and family histories
– Perform a pelvic examination
– Suggest imaging tests or referrals if needed
– Discuss genetic testing for those with hereditary risk factors
Prompt assessment enhances prospects for early detection and tailored treatment strategies.
When High-Risk Women Should Seek Advice
Women with a strong family history, BRCA mutations, or hereditary cancer syndromes should consult a specialist regarding:
– Regular monitoring
– Preventive measures
– Tailored screening recommendations
Proactively managing risk is a vital aspect of health maintenance.
Prevention and Risk-Management Tips
While ovarian cancer cannot always be avoided, women can take proactive measures to manage risk, support early detection, and safeguard long-term health. These steps emphasize awareness, lifestyle choices, and educated medical decisions.
Practical Risk-Management Guidelines
– Know your family history—discuss any cases of ovarian, breast, or colorectal cancer with your doctor.
– Consider genetic counseling if a strong family history or suspected hereditary risk exists.
– Schedule routine gynecological examinations and report persistent symptoms promptly.
– Achieve a healthy weight through balanced diets and regular exercise.
– Avoid smoking and limit alcohol consumption.
– Discuss hormone therapy risks with your healthcare provider before or during menopause.
– Make informed decisions regarding reproductive and contraceptive options in consultation with a medical practitioner.
Risk management focuses on awareness and prevention-driven decisions, not anxiety or fear.
Frequently Asked Questions (FAQs)
- Can ovarian cancer be hereditary?
Yes. Inheritable gene mutations like BRCA1, BRCA2, and Lynch syndrome significantly increase ovarian cancer risk. Women with substantial family history should consider genetic counseling and testing.
- Does birth control usage increase or decrease ovarian cancer risk?
Most evidence suggests that oral contraceptives lower ovarian cancer risk by reducing lifetime ovulation. Yet, contraceptive choices should always be discussed with a healthcare provider.
- Can lifestyle changes fully prevent ovarian cancer?
No. While lifestyle changes cannot entirely prevent ovarian cancer, a healthy weight, regular activity, avoiding tobacco, and a balanced diet may help lower overall risk.
- Who should think about genetic testing for ovarian cancer risk?
Women with a family history of ovarian, breast, or colorectal cancer—particularly among first-degree relatives—or those with known family genetic mutations should consult a genetic counselor.
- Are there screenings for ovarian cancer?
Currently, there is no standardized screening test for ovarian cancer in women at average risk. However, high-risk individuals may undergo routine transvaginal ultrasounds and CA-125 blood tests under medical supervision.
- Does age influence ovarian cancer risk?
Yes. Risk escalates after age 40, with most diagnoses occurring post-menopause. Age is one of the major non-modifiable risk factors.
- Can pregnancy or breastfeeding diminish ovarian cancer risk?
Yes. Both pregnancy and breastfeeding reduce the number of ovulation cycles, correlating with lower risk levels. Multiple pregnancies might offer extended protection.
- Are hormone replacement therapies (HRT) connected to ovarian cancer?
Long-term use of estrogen-only HRT, especially post-menopause, might slightly heighten risk. Women should weigh the benefits and drawbacks of HRT with their healthcare providers.
- Do endometriosis or PCOS elevate ovarian cancer risk?
Certain studies suggest that endometriosis might increase vulnerability to specific ovarian cancer subtypes. PCOS may also link to heightened risk due to hormonal imbalances, although evidence is still being developed.
- Which symptoms should prompt medical evaluation?
READ ALSO: At What Age Does Menopause Begin?
Persistent or unusual symptoms lasting over two weeks should be evaluated by a doctor, including:
– Abdominal bloating or swelling
– Pelvic or lower abdominal discomfort
– Loss of appetite or rapid fullness
– Frequent urination
– Unexplained fatigue or back pain
Early evaluation can enhance detection and treatment success.
Conclusion
Understanding ovarian cancer‘s causes and chief risk factors is essential for promoting awareness, making informed choices, and pursuing proactive medical care. While many risks—such as age and genetics—cannot be controlled, women can lessen uncertainty by exploring their family history, seeking timely medical advice, and making health-focused decisions.
Awareness does not eradicate risk, but it empowers women to identify warning signs earlier, engage in proper screening when needed, and take charge of their reproductive health for the long
term.






