When Does Ovulation Occur? 7 Essential Facts Every Woman Should Know
Introduction
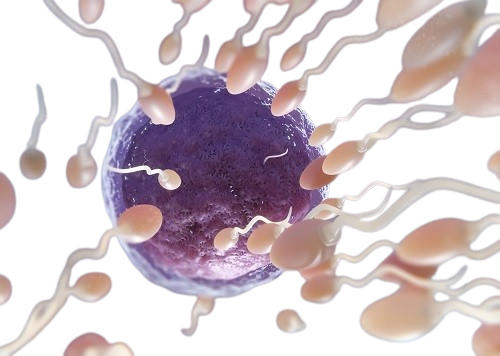
Knowing when you ovulate is crucial for enhancing fertility and reproductive health. Whether your goal is to conceive, prevent pregnancy naturally, or better understand your cycle, aware timing of ovulation can greatly impact your efforts. Ovulation meaning: Ovulation represents a key moment in the menstrual cycle—when a mature egg is released from the ovary, awaiting fertilization.
This event generally occurs once per cycle, yet the timing may vary among women and fluctuate monthly. Grasping the timing of ovulation is crucial for effective pregnancy planning or managing reproductive aims. In this article, we’ll explore 7 essential facts about ovulation, including how to identify it, factors influencing its timing, and how to monitor it effectively for improved health and fertility.
When Does Ovulation Occur? : It Usually Takes Place in the Middle of the Menstrual Cycle
A commonly accepted notion is that ovulation happens around the middle of the menstrual cycle. This period signifies the release of a mature egg and is considered the most fertile time for women. While this guideline is applicable to many, recognizing the details of when and how ovulation occurs can significantly enhance your fertility tracking—especially if your cycle is irregular.
Decoding the Menstrual Cycle
To determine when ovulation occurs, it’s helpful to break the menstrual cycle into three primary phases:
1. Follicular Phase (Day 1 to Ovulation): Starts on the first day of your period. In this phase, hormones promote the growth of follicles within the ovaries, one of which matures into an egg. Estrogen levels increase, and the uterine lining begins to thicken.
2. Ovulation (Mid-Cycle): Triggered by a sharp increase in luteinizing hormone (LH), typically around day 14 in a 28-day cycle. The mature egg is released into the fallopian tube, where it can be fertilized.
3. Luteal Phase (Post-Ovulation to Day 28): Once the egg is released, the empty follicle transforms into the corpus luteum, generating progesterone to prepare the uterine lining for potential pregnancy. If fertilization doesn’t take place, hormone levels decline, leading to menstruation.

What Does “Midway” Really Signify?
The term “midway” generally refers to the middle of the menstrual cycle—around day 14 in a standard 28-day cycle. Nonetheless, this is an average and not a strict rule. Ovulation doesn’t always occur on day 14 for everyone; it depends on:
Cycle Length: Not all women have a 28-day cycle. Some may have shorter (e.g., 24 days) or longer cycles (e.g., 32 days).
Luteal Phase Stability: The luteal phase (following ovulation) tends to be consistent—around 12 to 14 days—meaning ovulation usually occurs 12 to 14 days before the onset of the next period, rather than exactly 14 days after the last period started.
Example:
-28-day cycle: Ovulation may happen around day 14.
– 30-day cycle: Ovulation often occurs approximately on day 16.
– 24-day cycle: Ovulation can happen as early as day 10.
Why This Matters
Recognizing that ovulation typically happens mid-cycle is vital for several key reasons:
1. Fertility Awareness: For those trying to conceive, timing intercourse in the days leading up to and including ovulation maximizes chances of pregnancy.
2. Natural Birth Control Techniques: Understanding when your ovulation occurs is crucial for methods like the fertility awareness method (FAM), which involves refraining from unprotected sex during fertile days.
3. Monitoring Reproductive Health: Irregular ovulation may signal underlying health issues such as PCOS, thyroid disorders, or hormonal issues. Recognizing expected ovulation timing helps identify irregularities.
Hormonal Signals That Govern Mid-Cycle Ovulation
During the cycle’s midpoint, hormonal shifts facilitate ovulation:
– Rising estrogen levels from the dominant follicle instruct the brain to release a surge of luteinizing hormone (LH).
– This surge is the catalyst that leads to the follicle rupturing and the egg being released, marking ovulation.
The LH surge usually happens 24 to 36 hours before ovulation, which is a useful marker in predicting imminent ovulation.
What If You’re Not Ovulating Mid-Cycle?
While mid-cycle ovulation is standard for many women, some may ovulate at different times or not at all. Possible causes include:
– Stress
– Traveling or jet lag
– Excessive physical activity
– Sudden weight fluctuations
– Polycystic Ovary Syndrome (PCOS)
– Perimenopause or menopause
– Thyroid issues
If you’re not experiencing signs of ovulation mid-cycle, using ovulation predictor kits, monitoring your basal body temperature, or consulting a healthcare professional may help clarify your situation.
When Does Ovulation Occur In A Woman?
Ovulation typically occurs around the cycle’s midpoint, about 12 to 16 days before your next period begins.
– Mid-cycle timing relies on the regularity and length of your cycle.
– Being aware of your ovulation pattern empowers you to make informed choices regarding your fertility, conception, and reproductive health.
Your Fertile Window Is Narrow — But Crucial
In terms of conception, timing is fundamental, and this is where your fertile window is critical. The fertile window consists of a short range of days in your cycle when the chances of conception are highest. While the entire menstrual cycle lasts roughly 28 to 35 days, the feasible time for conceiving is considerably shorter, approximately 6 days.
Despite its brevity, this window is vital for women aiming to conceive and equally important for those wanting to prevent an unwanted pregnancy naturally. Understanding this window enhances informed decisions about your reproductive health.
Menstruation Cycle Phases: What Constitutes the Fertile Window?
The fertile window involves the five days leading up to ovulation plus the day of ovulation itself. This is when sperm and egg have the opportunity to unite, resulting in fertilization.
Overview of the 6-Day Fertile Window:
-Days -5 to -1 before Ovulation: Sperm can live in the female reproductive tract for up to 5 days, so if you engage in sexual activity during this timeframe, the sperm may still be viable when the egg is released.
– Day of Ovulation: The mature egg is released and remains viable for 12 to 24 hours, marking peak fertility.
– Day After Ovulation:
Some specialists include this day within the window, although the egg is generally no longer viable.
Menstruation Cycle Phases: Why Is the Fertile Window Important?
Your likelihood of conception is highest when intercourse occurs during your fertile window, specifically within the two days before ovulation and on ovulation day itself.
Conception Odds:
– 5 days before ovulation: 10% chance of pregnancy
– 2 days before ovulation: ~25–30% chance
– On ovulation day: ~30–35% chance
– 1 day after ovulation: Drops significantly to ~10% or less
– 2 days post-ovulation: Nearly 0% chance
This highlights the necessity of timing intercourse accurately within this window for couples seeking to conceive.
When Does Ovulation Occur? And How to Determine Your Fertile Window
Given the limited duration of the fertile window and its slight monthly variations, diligently tracking your cycle is critical. Here are several methods to assist in identifying it:
1. Cervical Mucus Observation: During fertile days, cervical mucus changes to a clear, stretchy, slippery consistency resembling raw egg whites, signaling that ovulation is near.
2. Basal Body Temperature (BBT) Tracking: Following ovulation, your body temperature slightly rises (approximately 0.5°F). Consistently charting your BBT can confirm ovulation has occurred and assist in predicting upcoming cycles.
3. Ovulation Predictor Kits (OPKs): These identify the LH surge that arises 24–36 hours before ovulation. A positive result indicates impending ovulation.
4. Fertility Tracking Apps: Digital applications analyze your cycle data to forecast your fertile window, particularly useful when symptoms are tracked consistently over time.
Menstruation Cycle Phases: -Common Pitfalls to Avoid
Even women with regular cycles may miscalculate their fertile window. Here are some pitfalls to watch for:
– Relying Solely on Calendar Apps: Apps provide averages but don’t account for your hormonal patterns.
– Assuming Ovulation Always Occurs on Day 14: This only applies to perfectly regular 28-day cycles.
– Neglecting Cervical Mucus Indicators: Daily checks are crucial, as you may miss fertile days without consistent observation.
Menstruation Cycle Phases: Tips for Maximizing Your Fertile Window for Conception
– Engage in intercourse every 1–2 days during your fertile window to ensure that healthy sperm are present when the egg is released.
– Use fertility-friendly lubricants to avoid harming sperm health.
– Maintain relaxation to minimize stress, as anxiety may disrupt ovulation timing.
Using the Fertile Window for Birth Control? Use Caution
Many utilize natural family planning (NFP) techniques to prevent pregnancy by avoiding sexual activities during the fertile window. However, this method requires precise and consistent tracking, and an inherent margin of error exists. If you’re not ready for pregnancy, employ backup methods like condoms or consult a healthcare professional about your alternatives.
Key Takeaways
– The fertile window encompasses about 6 days, including the 5 days before ovulation and the day of ovulation itself.
– The likelihood of conception peaks in the 2 days leading up to ovulation and on ovulation day.
– Learning to recognize and monitor your fertile window can vastly improve your chances of conceiving or assist in natural pregnancy avoidance.
– Combining tracking methods enhances accuracy, especially for those with irregular cycles.
Physical and Hormonal Indicators Suggest Ovulation Is Approaching
Your body is incredibly adept at signaling when it’s most fertile, provided you know what to observe. As ovulation nears, various physical and hormonal shifts take place to ready your body for potential conception. Identifying these indicators can help you naturally determine your fertile window and enhance your chances of pregnancy—or prevent it, if that’s your intention.
These signs stem from a subtle interplay of reproductive hormones, and grasping them can enhance your understanding of your cycle’s health.
Hormonal Changes Involved in Ovulation
Ovulation isn’t random; it’s governed by a sequence of hormonal transformations throughout your menstrual cycle. The two primary hormones are:
– Estrogen: Levels rise as the follicle develops, aiding in uterine lining thickening and preparing your body for ovulation. Increasing estrogen also stimulates the creation of high-quality cervical mucus.
– Luteinizing Hormone (LH): A sharp surge (LH surge) occurs 24 to 36 hours before ovulation, prompting the release of the mature egg from the ovary.
By monitoring these hormonal variations—either through symptoms or ovulation test kits—you can accurately forecast when ovulation will take place.
Menstruation Cycle Phases: -Common Physical Indicators Signaling Imminent Ovulation
Here are some reliable physical clues that indicate you may be ovulating or close to ovulation:
1. Cervical Mucus Alterations
Cervical mucus experiences significant transformations during your cycle:
– Dry or sticky mucus = low fertility (before or after ovulation)
– Creamy or lotion-like mucus = approaching ovulation
– Clear, stretchy, and slippery (resembling egg whites) = high fertility; ovulation is imminent or occurring
This fertile mucus facilitates sperm movement through the cervix toward the egg.
2. Increased Sex Drive
Many women report heightened sexual desire or attractiveness during ovulation. This is nature’s method of increasing reproductive chances during peak fertile times.
3. Mild Pelvic or Abdominal Discomfort (Mittelschmerz)
Some women may experience a slight ache or sharp twinge on one side of the lower abdomen around ovulation, known as mittelschmerz—a term meaning “middle pain.” This sensation usually lasts from a few minutes to several hours.
4. Breast Sensitivity
Hormonal changes, particularly progesterone rise after ovulation, can lead to breast tenderness. This is a typical post-ovulation indication that ovulation has occurred.
5. Enhanced Senses
Some women notice heightened senses of smell, taste, or sight around ovulation due to hormonal shifts.
6. Light Spotting
Occasionally, a small amount of light pink or brown spotting may happen during ovulation. This can result from the egg breaking through the follicle or hormonal fluctuations influencing the uterine lining.
7. Cervical Position Changes
For those comfortable checking, the cervix rises, softens, and opens during ovulation. When not in the fertile window, it typically appears lower, firmer, and closed.
Menstruation Cycle Phase: -Confirming Ovulation with Hormone-Based Methods
If you’re uncertain about physical signs, hormone-based methods can more accurately detect ovulation:
Ovulation Predictor Kits (OPKs)
These kits test your urine for LH surges. A positive reading suggests ovulation will likely occur within the next 24–36 hours.
Basal Body Temperature (BBT) Monitoring
After ovulation, progesterone triggers a slight increase in resting body temperature (about 0.5°F or 0.3°C). Daily BBT tracking can help you confirm that ovulation has already occurred, though it doesn’t predict it.
Saliva Microscopes
These devices identify estrogen surges in saliva before ovulation. When estrogen levels peak, a fern-like pattern appears under the microscope.
When Does Ovulation Occur? -Importance of Recognizing These Symptoms
Being aware of your body’s ovulation signs offers numerous advantages:
– Helps time intercourse for conception
– Aids in natural birth control (fertility awareness method)
– Enhances menstrual cycle tracking accuracy
– Identifies potential cycle issues, such as anovulation (lack of ovulation)
If you never experience these indicators or notice sudden changes, it may suggest an underlying hormonal imbalance or ovulation disorder, which should be addressed with a healthcare professional.
Key Points to Remember For Menstruation Cycle Phase
Distinct physical and hormonal signs signal ovulation that you can monitor.
– Changes in cervical mucus, LH surges, and mild abdominal discomfort are common indicators.
– Ovulation predictor kits and BBT tracking are useful tools for confirming ovulation.
– Observing and understanding these signs empowers you to make informed reproductive health decisions.
Tracking Ovulation Through Various Reliable Approaches
If you’re trying to conceive or simply wish to gain insight into your reproductive health, tracking ovulation is one of the most effective strategies at your disposal. While your body often signals subtle signs of ovulation, employing reliable tracking methods can eliminate uncertainty and provide accurate information about your most fertile periods.
Multiple established techniques are available to facilitate your ovulation monitoring. You can choose from high-tech options or prefer natural methods to find what suits you best.
1. Ovulation Predictor Kits (OPKs)
OPKs are among the most convenient and accurate tools to detect impending ovulation. These over-the-counter urine tests identify the luteinizing hormone (LH) surge that typically occurs 24 to 36 hours prior to egg release.
– Pros: Easy to use, over 99% accuracy, widely accessible.
– Cons: Can be costly for daily usage and may not yield reliable results for women with hormonal imbalances like PCOS.
Tip: For optimal results, use OPKs in the morning and begin testing several days before anticipated ovulation.
2. Basal Body Temperature (BBT) Charting
BBT tracking involves measuring your temperature first thing each morning before getting out of bed. Following ovulation, progesterone causes a slight rise in basal body temperature, usually by 0.3–0.5°C (0.5–1.0°F).
– Pros: Inexpensive, natural, effective for confirming ovulation.
– Cons: Cannot predict ovulation ahead of time; only verifies it afterward.
Tip: Utilize a digital basal thermometer and record your results daily over at least 2–3 cycles to observe patterns.
3. Cervical Mucus Tracking
Monitoring cervical mucus changes is a natural, effective approach to estimate your fertile window. As ovulation nears, mucus becomes clear, stretchy, and slippery—similar to raw egg whites—helping sperm navigate through the cervix towards the egg.
– Pros: Free, hormone-free, beneficial for predicting and confirming ovulation.
– Cons: Requires consistent daily observation and may be initially unclear.
Tip: Check cervical mucus daily after using the bathroom and note the texture and color in a tracking app or journal.
4. Saliva Ferning Microscopes for Hormone Tracking
Some women use saliva microscopes to identify rising estrogen levels before ovulation. When estrogen peaks, dried saliva forms a crystalline “ferning” pattern under a microscope, indicating that ovulation is likely approaching.
– Pros: Reusable and non-invasive.
– Cons: Learning to interpret patterns may take time.
Tip: Refrain from brushing your teeth, consuming food, or drinking before testing your saliva.
5. Fertility Tracking Applications
Mobile applications like Flo, Clue, Natural Cycles, Premom, and Kindara assist you in logging menstrual symptoms, basal temperature, OPK results, and cervical mucus alterations. Some leverage advanced algorithms or integrate with digital thermometers or wearable sensors.
– Pros: Convenient, aids in spotting patterns over time, and many are free.
– Cons: Accuracy hinges on consistency and data input.
Tip: Select an app that allows for customization and compatibility with ovulation devices, if you’re using them.
6. Progesterone Blood Tests
You can request a progesterone blood test (usually performed around day 21 of your cycle) to verify whether ovulation has taken place. Progesterone levels typically rise post-ovulation and are crucial for early pregnancy.
– Pros: High medical accuracy, beneficial for fertility assessments.
– Cons: Involves lab visits and may not be practical for routine tracking.
7. Cervical Position Monitoring
Some advanced fertility trackers evaluate the cervix’s position. During ovulation, the cervix becomes softer, elevated, and more open.
– Pros: Natural and no cost involved.
– Cons: Requires practice and may be awkward for some individuals.
Tip: Always ensure your hands are clean, and check at the same time each day.
Final Thoughts: Choose What Suits You Best
The ideal ovulation tracking approach depends on your goals, lifestyle, and comfort level. Many women combine methods—for instance, utilizing OPKs along with BBT tracking—to enhance accuracy.
Whether your aim is conception, avoiding pregnancy, or simply achieving a better understanding of your cycle, tracking ovulation enables you to take charge of your reproductive health.
When Does Ovulation Occur in A Woman? Ovulation Timing Varies for Each Woman—and Month to Month
Ovulation does not adhere to a uniform schedule for all women and can shift even for the same woman from month to month. While a common belief suggests that ovulation typically occurs around day 14 of a 28-day cycle, this is more of a rough guideline than a definitive rule.
Menstruation Cycle Phase: Factors Influencing Ovulation Timing
Various internal and external influences can affect the timing of ovulation, including:
– Cycle Length: Those with longer or shorter menstrual cycles will not ovulate on the same day as those with a typical 28-day cycle. For instance, a woman with a 35-day cycle may ovulate closer to day 21, rather than day 14.
– Hormonal Changes: Fluctuations in hormones, particularly estrogen and luteinizing hormone (LH), significantly impact when ovulation occurs.
– Age: As women age, their cycles may become less reliable, particularly during the perimenopausal phase.
– Stress and Lifestyle Factors: Emotional stress, sudden weight changes, illness, or intense physical activity can delay or inhibit ovulation in any given month.
– Medical Conditions: Disorders like polycystic ovary syndrome (PCOS) or thyroid issues can lead to irregular or absent ovulation (anovulation).
Women with irregular menstrual cycles often face challenges in pinpointing ovulation. In these cases, monitoring ovulation signs or employing ovulation prediction tools can be especially beneficial. Additionally, it’s common for ovulation to vary slightly each month, even for those with regular cycles. This means that ovulating on day 14 one month and day 16 or 12 the next is completely normal.
Menstruation Cycle Phases: -What If Ovulation Doesn’t Happen?
Occasionally, women may experience months without ovulation, known as anovulation. This can occur due to:
– High levels of stress
– Inadequate nutrition
– Overexercising
– Hormonal imbalances
– Some medications
– Chronic health issues
Missing ovulation sporadically is typically normal, but consistent anovulation may suggest deeper concerns affecting fertility. If you have worries about irregular or absent ovulation, consulting a healthcare professional or fertility expert is advisable.
Key Takeaway
Recognizing that ovulation timing is not rigid can alleviate anxiety and dispel misunderstandings. Rather than relying solely on a universal cycle calendar, women should track their bodies and patterns using ovulation monitoring techniques to gain a clearer understanding of their fertility window.
When Does Ovulation Occur? -Hormones Are Central to Triggering Ovulation
Ovulation follows a meticulously controlled process influenced by a balance of hormones. Understanding their functions can clarify the timing of ovulation and factors that may cause shifts.
The Brain-Ovary Link
The hypothalamus, located in the brain, serves as the body’s fertility command center. It communicates with the pituitary gland, which signals the ovaries to prepare an egg for release.
Here’s a breakdown of the hormonal sequence:
1. Follicle-Stimulating Hormone (FSH) – The Egg Catalyst
Early in the menstrual cycle (typically around days 1–5), the pituitary gland produces FSH, prompting the ovaries to develop follicles—small fluid-filled sacs, each housing an immature egg. Generally, one of these follicles becomes the leading one and progresses toward maturity.
2. Luteinizing Hormone (LH) – The Ovulation Activator
With increasing estrogen levels from the growing follicle, a signal is sent to the pituitary to release a surge of LH. This LH surge directly initiates ovulation, leading to the release of the mature egg from the dominant follicle, typically occurring within 24 to 36 hours post-surge.
3. Estrogen – The Cycle Influencer
Estrogen levels rise in the first half of the cycle, helping to thicken the uterine lining in preparation for potential pregnancy. It also aids in changing cervical mucus, facilitating sperm movement toward the egg at ovulation time.
4. Progesterone – The Post-Ovulation Guardian
Following ovulation, the ruptured follicle transforms into the corpus luteum, which secretes progesterone. This hormone maintains the uterine lining and supports early pregnancy if fertilization occurs. If fertilization does not happen, progesterone levels drop, triggering menstruation and starting a new cycle.
Menstruation Cycle Phases And The Consequences of Hormonal Imbalance
Any disruption in this hormonal pathway can hinder or prevent ovulation. Common reasons for hormonal imbalances include:
– Polycystic ovary syndrome (PCOS)
– Thyroid conditions (hypothyroidism or hyperthyroidism)
– Elevated stress levels affecting the hypothalamus
– Extreme exercise or low body weight
– Certain medications
If ovulation disruptions occur due to hormonal imbalance, fertility and cycle health may be impacted. Hormonal testing from a healthcare professional can help identify potential issues and guide appropriate treatment.
Key Takeaway
Hormones are crucial in driving the ovulation process. From FSH and LH to estrogen and progesterone, each plays a significant role in reproduction. Monitoring hormone patterns—especially the LH surge—can assist women in better understanding their cycles and accurately determining their fertile windows.
READ ALSO: 5 Easy Ways to Calculate Ovulation Days After Menstruation
Ovulation Disorders: A Leading Cause of Infertility
Ovulation is critical for conception; if a woman does not ovulate consistently, her chances of becoming pregnant significantly decrease. Ovulation disorders are among the most prevalent causes of female infertility, representing approximately 25–30% of all infertility cases.

What Are Ovulation Disorders?
Ovulation disorders encompass conditions where ovulation occurs infrequently (oligo-ovulation) or not at all (anovulation). These issues may arise from hormonal imbalances, lifestyle influences, or underlying health concerns. Women with such disorders may experience irregular cycles, very long or short periods, or absence of periods entirely.
Common Types of Ovulation Disorders
1. Polycystic Ovary Syndrome (PCOS)
PCOS is the most frequent cause of ovulatory infertility, characterized by:
– Irregular or absent ovulation
– Elevated androgen levels (male hormones)
– Multiple small follicles in the ovaries as seen on ultrasound
2. Hypothalamic Amenorrhea
This condition arises from disruptions in communication between the brain and ovaries, often caused by:
– Stress
– Significant weight loss
– Overexercising
3. Premature Ovarian Insufficiency (POI)
Also referred to as early menopause, POI happens when the ovaries stop functioning properly before age 40, leading to irregular or absent ovulation.
4. Hyperprolactinemia
Elevated prolactin levels (the hormone associated with milk production) can hinder ovulation and may result from medications or issues with the pituitary gland.
5. Thyroid Disorders
Both hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid) can disrupt the hormonal balance required for ovulation.
How Are Ovulation Disorders Diagnosed?
A healthcare provider may use various methods to identify ovulation issues:
– Menstrual history: Irregular or missing periods can indicate potential issues.
– Hormone blood tests: Assessing levels of FSH, LH, estrogen, prolactin, thyroid hormones, and androgens.
– Ultrasound: Monitoring follicle development and identifying signs of PCOS.
– Basal body temperature and ovulation test kits: Used to track if and when ovulation occurs.
Can Ovulation Disorders Be Treated?
Absolutely! Many ovulation disorders can be managed through medical interventions and lifestyle adjustments:
– Medications: Agents like clomiphene citrate (Clomid) or letrozole can foster ovulation; sometimes, injectable hormones may be necessary.
– Lifestyle changes: Weight control, stress management, and improved nutrition can help restore regular ovulation, particularly in cases like hypothalamic amenorrhea or PCOS.
– Surgery: In certain cases of PCOS, ovarian drilling may enhance ovulation.
– Hormone therapy: Thyroid medications or treatments to lower prolactin can correct hormonal imbalances affecting ovulation.
Key Takeaway
If you’re having difficulty conceiving, an ovulation disorder might be the underlying cause—but the positive news is that many of these conditions are highly manageable with proper medical guidance. Recognizing the signs and seeking early diagnosis and treatment can greatly enhance your chances for a successful pregnancy.
Conclusion: When Does Ovulation Occur In A Woman?
Ovulation is a crucial component of reproductive health, whether you’re aiming for pregnancy or simply seeking a better understanding of your body. By learning when ovulation occurs, tracking your unique signs and patterns, and comprehending the hormonal dynamics at play, you equip yourself with valuable insight that can improve both your health and fertility outcomes.
These seven essential facts form the basis for better fertility planning and heightened cycle awareness. If you have uncertainties about your ovulation timing or experience irregularities, seeking professional help is a worthwhile step. Your health is truly invaluable.
Frequently Asked Questions About When Does Ovulation Occur?
1. When do women typically ovulate during their periods?
Most women ovulate about 14 days before their next period, rather than 14 days post their last period. For those with a standard 28-day cycle, ovulation generally takes place around day 14, though this can differ based on individual cycle length and consistency.
2. Is it possible to conceive outside of your ovulation period?
Conception is most probable during the fertile window, which spans the day of ovulation and the five preceding days. Nevertheless, since sperm can survive in the reproductive system for up to five days, intercourse before ovulation can still lead to pregnancy.
3. What is the duration of ovulation?
The act of ovulation — where the egg is released — is a short-lived occurrence, but the fertile window spans about 5 to 6 days, with maximum fertility observed the day before and on the day of ovulation.
4. What are the signs that indicate ovulation is happening?
Typical signs of ovulation include:
– Clear, stretchy cervical mucus resembling egg whites
– A slight increase in basal body temperature
– Mild pelvic discomfort or cramps (mittelschmerz)
– Increased sexual desire
– Soreness in the breasts
– A positive result on an ovulation predictor kit (OPK)
5. Is it possible to ovulate multiple times within a single cycle?
You can release more than one egg simultaneously (as seen with fraternal twins), but this generally occurs within a single 24-hour period. Ovulation does not happen at completely separate times within one cycle.
6. Does ovulation occur at the same time every month?
Not necessarily. Ovulation timing can slightly vary from month to month due to factors like stress, illness, travel, hormonal fluctuations, or changes in lifestyle, particularly in women who have irregular cycles.
7. What methods can I use to accurately track my ovulation?
You can monitor ovulation using the following:
– Ovulation predictor kits (OPKs)
– Basal body temperature (BBT) charts
– Observations of cervical mucus
– Ovulation tracking apps
– Fertility monitors
Using a combination of these approaches can enhance accuracy.
8. On which cycle day is ovulation typically most likely?
In a classic 28-day cycle, ovulation usually transpires on day 14. However, in longer or shorter cycles, it can happen anytime between days 11 and 21, based on the individual’s unique pattern.
9. Can factors like stress or illness postpone ovulation?
Absolutely. High levels of stress, illness, intense physical activity, or sudden weight changes can interfere with hormone signals between the brain and ovaries, thereby delaying or inhibiting ovulation.
10. What steps should I take if I’m not ovulating?
If you suspect you’re not ovulating or have irregular cycles, consider:
– Consulting a healthcare provider or a fertility expert
– Getting hormone levels evaluated (FSH, LH, estrogen, prolactin, thyroid)
– Addressing any underlying issues such as PCOS, thyroid problems, or lifestyle influences
– Exploring ovulation-inducing medications if you’re trying to conceive.
Watch, comment, and subscribe to our YouTube Channel https://www.youtube.com/@homecurestv1821/featured
Originally posted 2025-07-18 17:27:04.






